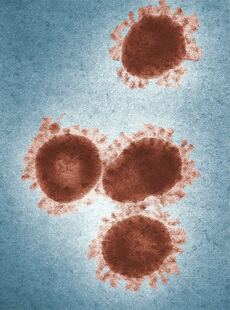
Chinese herbs in coronavirus treatmentTRADITIONAL CHINESE HERBAL REMEDIES As evidenced by a February 18th tweet from China Xinhua News, healthcare practitioners across China are relying on centuries-old remedies to treat the novel coronavirus. In the absence of targeted drugs and vaccines, with continual updates to the national diagnosis and treatment program for novel coronavirus, the role of traditional Chinese medicine (TCM) is on the rise. More COVID-19 patients are being treated with Chinese medicine or integrated Western-Chinese medicine, and the role of TCM herbal prescription formulas is expanding. What formulas are they using? What do the properties of these herbs tell us about TCM approaches to the virus? USE OF CHINESE HERBS TO TREAT THE CORONAVIRUS With an array of treatment methods and a wealth of experience in its arsenal, Chinese medicine has been used to fight plagues and epidemics for thousands of years. The focus of TCM is not just the virus itself but also symptoms and changes to the body caused by the invasion of the virus. Treatment starts with the patient as a whole, to identify patterns and then dispel sickness and support health. HERBAL FORMULA USAGE RATES 80% TO 95% Reports from throughout China indicate TCM formula usage rates of 80% to 95% in confirmed cases of novel coronavirus. One specialist described isolation wards containing a mix of mild, typical, and severe cases of novel coronavirus. Typical cases are characterized as imaging findings in the lungs but the absence of disease progression to respiratory failure. In hospitals, traditional Chinese medicine plays a significant role in regulating diarrhea, constipation, and other gastrointestinal symptoms; in addition, intervention with Chinese medicine may stop the condition from progressing to the severe and critical stages. WHAT FORMULAS ARE BEING USED? WHAT FORMULAS HAVE BEEN VALIDATED? 清肺排毒汤 The National Health Commission and the State Administration of Traditional Chinese Medicine recommend Qing Fei Pai Du decoction (清肺排毒汤); clinical observation and data analysis have been performed on the therapeutic efficacy of this classical TCM formula. One formula for Qing Fei Pai Du decoction appearing on multiple sites, including Baidu, listed 21 ingredients. The top ingredients in terms of quantity are calcium sulfate, Radix bupleuri (common name bupleurum, effective in the treatment of alternating chills and fever; may induce headache or nausea), Poria cocos (efficacy in draining dampness and transforming phlegm; concurrent administration of diuretics contraindicated), Radix dioscoreae (Chinese yam, known to tonify qi and yin of the lungs, spleen, and stomach; may have hypoglycemic effects, use with caution in comorbid hepatobiliary disease). 肺炎一号 Pneumonia Formula No. 1 (肺炎一号), developed by the Chinese Medicine Department at Guangzhou Eighth People's Hospital, and its variations Pneumonia Formula No. 2, Pneumonia Formula No. 3, Pneumonia Formula No. 4, and Pneumonia Formula No. 5 are also in use. Formula No. 1 has achieved favorable clinical results in Guangzhou. Formula No. 1 includes two herbs that clear heat and relieve toxicity, Flos lonicerae (honeysuckle flower) and Fructus forsythiae (forsythia fruit), along with 16 other ingredients. VARIATIONS In Chinese medicine, the treatment regimen adopted varies by person. If a patient is in poor physical condition, dispelling disease is not enough, treatment must focus on supporting health. For example, in those with poor appetite it is necessary to focus on spleen health; in patients with damp-heavy qi and thick tongue coating it is necessary to improve the flow of urine. Ear needling (acupuncture) may be used to treat the patient’s psychological state and resolve issues of insomnia, in order to restore the patient’s biological clock. Just as treatment varies by individual patient, the virus varies by region. This too is a factor in treatment selection. It would not be appropriate to select one uniform formula for the entire nation. NOT ADVOCATED FOR THE HEALTHY NOT ADVOCATED FOR THE PREVENTION OF CORONAVIRUS According to the head of a university of traditional Chinese medicine, the entire populace does not need to take this medicine. Healthy people need to improve resistance in order to avoid getting sick. High-risk populations, including healthcare providers, may take herbal remedies as appropriate. Practitioners emphasized that these are treatment prescriptions and are not recommended as preventive prescriptions. The general public should not self-administer these prescriptions. This blog briefly examines TCM principles and herbal remedies in light of recent Chinese media reports on novel coronavirus treatment in China. This examination is not intended to replace medical advice from a trained and qualified professional, and the use of herbal preparations is not recommended without the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity.
0 Comments
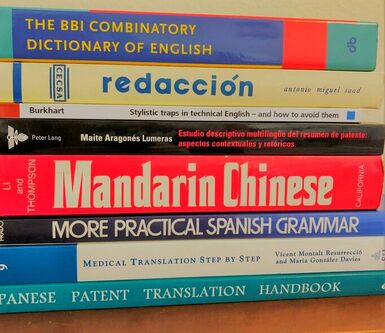
COMMON MISTAKES IN CHINESE-TO-ENGLISH TRANSLATION AND HOW TO ENSURE TRANSLATION QUALITY
What's the solution? Hire an experienced translator to ensure accurate translations. The standard in the translation industry is to translate into one's native language, thus a native English speaker is the best choice for Chinese-to-English translations. Look for a language professional with relevant language training, professional experience, and excellent written English. Grammatical errors and typos are red flags!
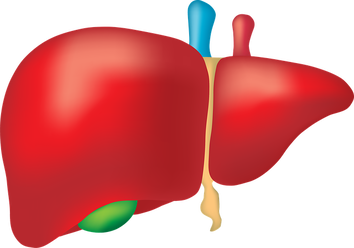
More questions about translation? Contact Integrative Translations. JANUARY 24TH UPDATE FROM THE CHINESE GOVERNMENT WEBSITEThe January 24, 2020, news update from the Health Emergency Response Office on the Chinese government website reported hundreds of confirmed cases of novel coronavirus nationwide and 25 deaths in Hubei Province and Hebei Province – an additional eight deaths compared to the January 23rd update, which detailed the anonymized medical histories of these initial 17 deaths. The majority were of advanced age (15 of the 17 over age 60), male (13 of 17), and suffered from such underlying conditions as liver cirrhosis, hypertension, cerebral infarction, diabetes, heart disease, chronic obstructive pulmonary disease, chronic renal insufficiency, Parkinson’s disease, and bronchitis. Most but not all presented with fever. Other symptoms at admission:
Novel coronavirus was confirmed through positive nucleic acid testing and monitored by electrocardiogram, lung CT, and blood-gas analysis. Therapies included oxygen, extracorporeal membrane oxygenation, endotracheal intubation (refused in some cases), anti-infectives, antibiotics, antipyretics, analgesics, and sedatives, supplemental fluids, and symptomatic therapies. Outcomes were intensifying respiratory failure, continuous declines in terminal oxygen saturation, reduced blood pressure, and ultimately death. Seven hospitals in Wuhan are offering intake for patients with high fever in order to identify new cases. How to tell if a document is written in Chinese, Japanese, or KoreanCHINESE VS JAPANESE VS KOREAN LANGUAGE Chinese, Japanese, and Korean all use characters, sometimes they use the same characters. While modern Japanese is a mix of kanji (Chinese characters) and the katakana and hiragana syllabaries, most of the time Korean is written in the Hangul alphabet, although I have seen older Korean documents written with Chinese characters. WHAT DOES CHINESE WRITING LOOK LIKE? Here are some clues to help you differentiate: Chinese characters are, in general, more complex. They look denser. A written Chinese character, whether traditional (Hong Kong, Taiwan) or simplified (China, Singapore), has more strokes than a Japanese or Korean character. WHAT DOES JAPANESE WRITING LOOK LIKE? Look for "no" (の). Look for dots(び). The Japanese language uses Chinese characters (kanji) and it uses two syllabaries (kana) of characters with only a few strokes. A Japanese document will contain multiple occurrences of the character “no” (の) which means “of” or denotes possession. So, glance through the document, do you see の scattered throughout? Then, it’s Japanese. Double dots also appear frequently, e.g., グ and ガ and ド. WHAT DOES KOREAN WRITING LOOK LIKE? I look for ovals. The Korean language has its own phonetic writing system, sometimes described as an alphabetic syllabary, and an oval shape appears frequently, for example, 여 and 우 and 으 and 어. You won’t see these oval shapes in Chinese. When you see a oval or circle shape in the Japanese language, it is a small circle パ. MORE EXAMPLES 敏捷的棕色狐狸跳過了懶狗 (traditional Chinese) 敏捷的棕色狐狸跳过了懒狗 (simplified Chinese) 빠른 갈색 여우는 게으른 개를 뛰어 넘는다 (Korean) 速い茶色のキツネは怠惰な犬を飛び越える (Japanese) WHAT ABOUT OTHER LANGUAGES AND OTHER WRITING SYSTEMS? จิ้งจอกสีน้ำตาลอย่างรวดเร็ว (Thai) cáo nâu nhanh (Vietnamese) хурдан бор үнэг (Mongolian) быстрая коричневая лиса (Russian) γρήγορη καστανή αλεπού (Greek) الثعلب البني السريع (Arabic) שועל חום מהיר (Hebrew) ፈጣን ቡናማ ቀበሮ (Amharic) Still have questions?
Write me at https://www.integrativetranslations.com/contact.html. I will look at your document and let you know. In the chill of winter, we gravitate to warmth and light.ASTRAGALUS Originating in northeastern China, central Mongolia, and Manchuria, the root of the herbaceous perennial Astragalus membranaceus or 黃芪 (huangqi) is a staple of traditional Chinese medicine. Mild in strength, with a sweet and slightly warm nature and an affinity for the spleen and lungs, astragalus is used as a general tonic to improve endurance, immune resistance, and energy, and to promote blood flow to the surface. Astragalus is useful for viral infections and increases the action of interferon alpha-1. It tonifies the spleen, the qi, and the blood. It is indicated for energy deficiency, fatigue, prolapse of rectum, womb, or other organs, profuse sweating due to external “empty” ailments, stubborn abscesses, facial swelling, and diabetes. The use of astragalus root as a general tonic dates to the 28th century BCE and the mythical Chinese ruler Shennong, the legendary author of the first materia medica. Astragalus root has a long, cylindrical taproot, which is internally yellowish in color, but rootlets should be absent. The constituents of astragalus root include triterpenoid saponins, astragalosides I-VIII, astramembranins I and II, isoglavones including formononetin and kumatakenin, and polysaccharides known as astrogaloglucans. There is anecdotal but little clinical evidence that astragalus alone or in combination aids in the treatment of the common cold or impaired immunity. Clinical studies supported by data from over 1000 patients in China confirm the use of astragalus as an immunostimulant for use in colds and upper respiratory infections. It is also used prophylactically. In general, astragalus is well tolerated but should probably be avoided in autoimmune diseases. WINTER TONIC SOUP Traditionally, the roots of Astragalus membranaceus are added to soup before the cold season to prevent respiratory ailments. Astragalus is an adaptogen and increases qi. The recommendation is to eat astragalus soup daily for one to three months to build immunity for the winter. INGREDIENTS Root herbs astragalus, ginseng, eleuthero Six cups low-salt soup broth 2 tablespoons olive oil 2 cloves garlic 4 carrots 1 onion 1-2 pounds chicken (optional - for added immunity) 2 cups of chopped greens (spinach, chard, kale) 4 sprigs of parsley 2-3 sprigs of sage 6 slices of ginger root Step 1: Soak root herbs in large pot with soup broth while preparing Steps 2 and 3. Step 2: Mince garlic, chop carrots and onion. Sauté in olive oil over low heat until onions are translucent. Step 3: Add chicken to above and brown on both sides. Step 4: Add sautéed carrots, onions, and garlic, as well as chopped greens, sprigs of parsley and sage, slices of ginger, and chicken to soup broth. Step 5: Simmer soup 3-4 hours, then remove root herbs, ginger slices, and sprigs of parsley and sage. Step 6: Season to taste with salt and pepper or soy sauce/hot oil/sesame oil. Information in this blog is presented for educational purposes only. The use of herbal preparations is not recommended without seeking the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity. In theory, astragalus may enhance the activity of drugs for diabetes and hypertension. Avoid astragalus root if you already have cold, flu, or fever.
Tips and advice on where to find a qualified professional translator for your business needs. A translator works with the written word and an interpreter works with the spoken word. Do you have a document requiring translation or do you need to schedule an interpreter for a court hearing, business negotiation, or medical appointment? Here's some advice on how to find a professional translator or interpreter. RECOMMENDATIONS Ask a trusted colleague in your industry for a referral to a translator or interpreter they work with regularly. If you know a qualified Spanish translator but need to have a document translated into French, ask the Spanish translator for a referral. Translators often network with one another and asking for a recommendation is a great place to start when looking for a professional translator. ONLINE SOURCES Search engines Use your preferred search engine to locate the websites of professional translators. Be specific: "English Italian interpreter" deposition "San Francisco" or "Chinese English translator" "journal articles." Professional translators' associations National and local translators' associations operate directories for their members which you can access for free. Here is a partial list of websites with specific links to search for a translator or interpreter.
National association American Translators Association Find a translator or interpreter Regional and local groups Association of Translators and Interpreters of Florida Find a professional Carolina Association of Translators and Interpreters Find a translator/interpreter Colorado Translators Association Directories > Translators and Interpreters Michigan Translators/Interpreters Network Find a Translator/Interpreter New Mexico Translators and Interpreters Association The Directory New York Circle of Translators Find a Linguist Northwest Translators & Interpreters Society Find a language specialist Oregon Society of Translators and Interpreters Find a translator/interpreter HELPFUL GUIDELINES
Still have questions? Contact me at https://www.integrativetranslations.com/ and I will do my best to help. Directory information provided as a public service for those seeking a dedicated professional to assist with translation or interpretation services for a given language. The inclusion of a particular directory does not denote endorsement of the information therein. An individual's inclusion in a particular association directory indicates only that said individual is a current member of the association.
Recent research on the hepatorestorative and hepatoprotective properties of active ingredients in traditional Chinese medicine Active ingredients in herbs from traditional Chinese medicine have shown promising efficacy in rehabilitating and protecting the liver after injury from excess acetaminophen. Drug-induced liver injury A significant number of cases of acute liver failure are caused by acetaminophen, also known as paracetamol. Acetaminophen is not toxic to the liver, but its reactive metabolite may cause liver injury. Excess quantities of acetaminophen can deplete the glutathione needed to convert the toxic metabolite NAPQI into a nontoxic metabolic product. Toxins generated during metabolization, mitochondrial dysfunction, inflammatory response, oxidative stress, the release of damage-associated molecular patterns (DAMPs), autophagy, endoplasmic reticulum stress, and microcirculatory dysfunction are among the mechanisms of injury. Limits of pharmacologic drugs The chief pharmacologic agent used for the clinical treatment of acetaminophen-induced liver injury is N-acetylcysteine (NAC), but NAC has limited treatment results and its administration is time-sensitive. For optimal results, NAC is administered approximately one hour after oral acetaminophen. Protective effects of traditional Chinese medicine A number of active ingredients discovered in Chinese herbs suppress liver toxicity. These compounds vary in how they benefit liver injury: they may alleviate liver disease, mitigate damage to liver tissue, reduce the degree of liver injury, and prevent or ameliorate side effects by suppressing the pathways and mechanisms of liver injury. These active ingredients are fast acting, with notable efficacy and few toxic side effects, and include polyphenol compounds, flavonoid compounds, saponins, organic acids, terpenoid compounds, phenylpropanoids, polysaccharides, and alkaloids. Polyphenol compounds Polyphenol compounds are widely present in traditional Chinese herbal remedies. Polyphenols can affect the production of biomarkers associated with oxidative stress, a major cause of hepatotoxicity induced by acetaminophen overdose. In the research of Hasanein (2017), rosmarinic acid (found in basil, rosemary, and lemon balm) produced remarkable hepatoprotective effects by inhibiting CYP2E1 activity in the liver and lipid peroxidation. Flavonoid compounds The protective effects of flavonoid compounds include the effects of ginseng anthocyanins on acetaminophen-induced hepatotoxicity (Qi 2017) and hyperoside which can hinder the formation of toxic intermediates and boost acetaminophen detoxification in the liver (Xie 2016). Fu (2018) discovered that α-mangostin notably suppressed acetaminophen-induced oxidative stress; α-mangostin, a xanthone derivative found in the pericarp of mangosteen fruit, also reduced inflammatory response through the anti-inflammatory mechanism mediated by the NF-κB and mitogen-activated protein kinase (MAPK) signaling pathways. Lu (2018) demonstrated that licochalcone A isolated from the root of Glycyrrhiza glabra had a protective effect on acetaminophen-induced liver injury through the Nrf2-mediated oxidative stress defense mechanism. Saponins Xu (2017) discovered that the antioxidant, anti-apoptotic, and anti-inflammatory actions of saponins (ginsenosides) had a protective effect on acetaminophen-induced liver injury in mice. Hu (2017) found that ginsenoside Rk1 pretreatment of acetaminophen-induced liver injury in mice significantly lowered levels of the lipid peroxidation product MDA. By increasing Bcl-2 and reducing Bax protein expression, ginsenoside Rk1 impeded activation of the apoptosis pathway. In Ning (2018), ginsenoside Rg1 prevented acetaminophen-induced liver injury through in vivo and in vitro activation of the Nrf2 signaling pathway. Leng (2018) proved that Platycodon grandiflorum saponins had pronounced protective effects on acetaminophen-induced liver injury through the NF-κB and AMPK/PI3K/Akt signaling pathways. Organic acids In Heidari (2016), taurine effectively relieved acetaminophen-induced liver injury and its complications in mice. Jiang (2017) established that, by reducing thiobarbituric acid reactive substances (TBARS) which form as a byproduct of lipid peroxidation and reducing iNOS, COX-2, TNF-2, IL-12, and IL-6, the acids from Potentilla chinensis inhibited inflammation and oxidative stress to alleviate acetaminophen-induced liver injury. Cha (2018) discovered that p-coumaric acid (an abundant isomer of hydroxycinnamic acid widely found in fruits and vegetables) suppressed acetaminophen-induced hepatocyte apoptosis by modulating the MAPK signaling axis in a reactive oxygen species (ROS)-dependent manner and by alleviating response and inflammation from ROS-mediated DNA damage . Terpenoid compounds In Uchida (2017), compounds in the essential oil of Cymbopogon citratus (lemongrass) hindered neutrophil migration and antioxidant activity in mice with acetaminophen-induced liver injury, thus relieving hepatotoxicity. The research of Zhang (2017) proved that by inhibiting the TNF-α-mediated JNK signaling pathway and the phosphorylation ERK and P38 pathways, pretreatment with astaxanthin (natural sources include shrimp, algae, yeast, and salmon) reduced hepatocellular necrosis, blocked the formation of ROS, prevented oxidative stress, and diminished cellular apoptosis, protecting the liver and alleviating drug-induced liver injury. In Yoshioka (2017), kamebakaurin (isolated from Rabdosia excisa) improved hepatotoxicity from acetaminophen overdose by inhibiting lipid peroxidation and inflammatory response in mice. Phenylpropanoids Fructus schisandrae (schisandra fruit) is widely used for liver protection in traditional Chinese medicine and the research of Jiang (2015) proved that lignan components in Fructus schisandrae ameliorated acetaminophen-induced liver injury by inhibiting acetaminophen's CYP-mediated biologic and metabolic pathways. Furthermore, in Jiang (2016) schisandrin B increased liver detoxification and antioxidation by activating the Nrf2/ARE pathway and regulating the Nrf2 target gene, reflecting its hepatoprotective effects. Yan (2018) demonstrated that, by activating sustained autophagy, glycycoumarin relieved acetaminophen-induced oxidative stress and thus prevented liver injury. Polysaccharides Lin (2018) found that polysaccharides of Dendrobium officinale played a hepatoprotective role by lowering oxidative stress and activating the Nrf2-Keap1 signaling pathway. And in Zhao (2018) the anti-inflammatory effects of polysaccharides of Coreopsis tinctoria regulated the expression of apoptosis-related proteins such as Bax and Bcl-2 to prevent acetaminophen-induced hepatotoxicity. Wu (2018) proved that polysaccharides of Poria cocos played a protective role against acetaminophen-induced liver injury in mice and their molecular mechanism was associated with suppression of the hepatocellular inflammatory response and apoptosis. Alkaloids Li (2014) discovered hepatoprotective effects of berberine on liver fibrosis via activation of AMP-activated protein kinase; and Zhao (2018) found that berberine had pronounced prophylactic effects on acetaminophen-induced hepatotoxicity by inhibiting oxidative stress, hepatocellular necrosis, and inflammatory response. In Park (2016), the alkaloids of Aconitum carmichaelii protected the organism against acetaminophen-induced injury by suppressing mitochondrial dysfunction and defending liver cells, although the herb is toxic when taken in excess. In 2018, a trial by Bian confirmed that ligustrazine (an alkaloid isolated from Ligusticum wallichii) improved acetaminophen-induced liver injury in mice by regulating the NF-κF and MAPK signal transduction pathways. Other compounds In Wangkheirakpam (2018), Auricularia delicata demonstrated antimicrobial, antioxidant, and protective effects on acetaminophen-induced liver injury in rats. In Guo (2018), Rhizoma pinelliae extract regulated bile acid transporter protein in mice with acetaminophen-induced liver injury. By activating Nrf2 and inhibiting NF-κB signal transduction, Garcinia cambogia extract played a protective role in acetaminophen-induced liver injury in mice (Ibrahim 2018). The antioxidant, anti-inflammatory, and anti-apoptotic actions of tannic acid demonstrated significant hepatoprotective effects on acetaminophen-induced hepatotoxicity in the work of Zhang (2017). Acetaminophen is a leading cause of drug-induced liver injury and recent research findings indicate that the use of active ingredients from traditional Chinese medicinal herbs might ameliorate such injury. Research on mechanisms of liver injury and the means by which such compounds protect against and alleviate injury holds promise for future antidotes to drug-induced liver injury. Please note: The herb information in this blog is presented for educational purposes only. The use of herbal preparations is not recommended without seeking the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity. Contact Integrative Translations for a full list of references. On November 5, 2019, the FDA updated its 2017 safety communication to remind patients, healthcare professionals, and laboratory technicians that levels of biotin or B-7, a B-complex vitamin and a common component of dietary supplements, higher than the recommended daily allowance may interfere with lab test results. Many dietary supplements promoted for hair, skin, and nails contain biotin levels up to 650 times the recommended daily intake of biotin. Physicians may also recommend high levels of biotin for patients with certain conditions such as multiple sclerosis. Biotin levels higher than the recommended daily allowance may cause interference with lab tests. In its most recent update, the FDA reminds the public, healthcare providers, lab personnel, and lab test developers that biotin, often found in dietary supplements, can cause clinically significant incorrect lab test results. The FDA has seen an increase in the number of reported adverse events, including one death, related to biotin interference with lab tests. Incorrect test results may lead to inappropriate patient management or misdiagnosis. Biotin in patient samples can cause falsely high or falsely low results, which may lead to inappropriate patient management or misdiagnosis. For example, a falsely low result for troponin, a clinically important biomarker to aid in the diagnosis of heart attacks, may lead to a missed diagnosis and potentially serious clinical implications. Consumers are advised to tell their doctor if they are taking biotin. Healthcare providers should talk to their patients about any biotin supplements they may be taking. Know that biotin is found in multivitamins – including prenatal multivitamins, biotin supplements, and dietary supplements for hair, skin, and nail growth – at levels that may interfere with lab tests. Lab personnel using assays with biotin technology must educate themselves and others about the potential for biotin interference. The recommended daily allowance of biotin is 0.03 mg and biotin is present in small amounts in many foods including whole grains, eggs, walnuts, avocados, egg yolk, liver, and yeast. Forms for healthcare professionals and patients to report safety information:
https://www.fda.gov/safety/medwatch-fda-safety-information-and-adverse-event-reporting-program/medical-product-safety-information FDA Safety Communication: https://www.fda.gov/medical-devices/safety-communications/update-fda-warns-biotin-may-interfere-lab-tests-fda-safety-communication Under the oaks and evergreens at 7420 feetWILD STRAWBERRY Wild strawberry runs along the trail. Tea of strawberry leaves and stems is valued for its mild astringent effects, and its antirheumatic, diuretic, antidiarrheal, tonic, and laxative properties. Strawberry is recommended in many traditions for intestinal sluggishness and for pregnancy, convalescence, and chronic stomach sensitivity when stronger herbs are contraindicated. WORMWOOD Known variously as 艾叶 (aiye), artemisia, or mugwort, wormwood is an intense bitter that stimulates underactive digestion and aids anemia. An anti-inflammatory and antidepressant, wormwood can be added as a potentiating factor to other preparations. Its active substances include essential oils, sesquiterpene lactones, azulenes, flavonoids, phenolic acids, and lignans. The whole plant is used as an antimalarial. Wormwood herbal tea is administered as a stomach stimulator and orexigenic. In Chinese medicine, wormwood warms the channels and stops bleeding. It dispels cold and alleviates pain, calms the fetus, resolves phlegm, and stops cough and asthma. As an aromatic, wormwood is used in sweat baths and saunas. Wormwood-juniper smudge sticks cleanse spaces and purge negativity. VERBENA The constituents of verbena or 马鞭草 (mabiancao, literally, horsewhip herb) include volatile oils, bitters, iridoids, alkaloids, mucilage, and tannins. It is a restorative, helpful for tension and long-term stress and good for convalescence from a long illness. The entire plant has sedative, tonic, diaphoretic, and anti-inflammatory properties and it is used to treat early-stage depression, melancholia, stress, and fever. Chinese medicine employs the bitter and cool properties of verbena to clear heat and remove toxicity, activate blood, disperse nodules, promote diuresis, and resolve swelling. It is indicated for jaundice caused by damp-heat, for fever due to external pathogens, and for dysmenorrhea or amenorrhea from blood stasis and abdominal masses. Its heat-clearing properties are used for severe sore throat and other accumulations of heat toxin including breast abscesses and swollen and painful gums. Extracts of lemon verbena and its major compound acteoside (ACT) have a regulatory effect on abnormal liver lipid metabolism; furthermore, ACT promotes lipolysis and fatty acid oxidation by increasing messenger RNA expression of adipose triglyceride lipase and carnitine palmitoyltransferase. OAK TREE The leaves, acorns, galls, and branches of oak trees contain tannin, quercetin, gallic acid, pectin, calcium, magnesium, and potassium. In various medical traditions, infusion of oak tree bark is administered internally to treat hemorrhoids, diarrhea, chronic dysentery, intestinal bleeding, and uterine bleeding, and, as a tea astringent, oak is applied externally to skin wounds, burns, mouth inflammation, toothaches, sore throats, and earaches. Oak gall possesses astringent, anti-inflammatory, antiviral, antidiabetic, larvicidal, antibacterial, and gastroprotective effects. Gallnuts have been sourced to produce drug therapies for cancerous diseases in traditional and folk medicine systems through the centuries, and the literature indicates that gallnuts contain a number of bioactive metabolites, accounting for their anticancer effects. Further screening of bioactive compounds is expected to yield valuable anticancer agents. JUNIPER The medicinal evergreen juniper or 杜松子(dusongzi) is resinous and aromatic. Internally, the leaves or berries have been used as a urinary antiseptic and for cystitis and urethritis, although juniper is contraindicated in people with kidney infection or chronic kidney weakness as the oils may be irritating to kidney inflammations. Juniper berries have diaphoretic and emmenagogue properties and the leaves have diuretic properties. In Chinese medicine, juniper works at the heart, spleen, and lung meridians and its key actions and medicinal uses include promoting digestion, warming the middle burner, expelling phlegm, warming the lungs, and cleansing the kidneys and liver. Topically, juniper is used to treat chronic skin irritations and as a relaxant. It relaxes the muscles and removes barriers to blood flow and energetic flow. Juniper is prized in many traditions for its ability to dispel tension and stagnation and the aromatic parts of the juniper plant have been employed as a protector against negativity. Juniper is known to have a stabilizing presence for those in need of safety and protection. Juniper's versatility extends to the culinary world and includes the flavoring of meat and sauerkraut and the distillation of gin. Please note: The herb information in this blog is presented for educational purposes only. The use of herbal preparations is not recommended without seeking the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity. Identifying local herbsBEAR CORN Bear corn or 肉苁蓉 (roucongrong) emerges from the soil under the oaks. A root parasite lacking chlorophyll, bear corn searches the dark soil to feed off the root system of the host tree. These New Mexico specimens are yellow and resemble ears of corn. In the words of Culpeper, “The juice or decoction of the young branches or seed, or the powder of the seed taken in drink, purgeth downwards and draweth phlegmatic and watery humors from the joints, whereby it helpeth the dropsy, gout, sciatica, and pains in the hips and joints.” Bear corn serves as an astringent, a poultice, a laxative, and a sedative. It restores strength, muscle tone, and balance after a long illness. In Chinese medicine, bear corn is a tonic to kidney-yang and a demulcent laxative; it tonifies yin as well as yang, lowers blood pressure, and is prized as an aphrodisiac and a uterine hemostatic. Modern research indicates that phenylethanoid glycosides isolated from bear corn may be effective in treating hot flashes and menopausal syndrome. YARROW The wet spring has produced a bumper crop of fernlike yarrow. Also known as thousand-leaf, yarrow is an important species in the traditional medicine of many cultures. It is antispasmodic, astringent, bitter, diaphoretic, and anti-inflammatory, and its constituents include coumarins, tannins, alkaloids, flavonoids, lactones, volatile oils, and triterpenes. Internally, yarrow is used to break fevers and to regulate the menstrual cycle, reduce heavy bleeding, and relieve menstrual pain. Externally, a salve or ointment of yarrow heals wounds and eases the pain of varicose veins. Yarrow has been used as a battlefield remedy for its ability to stanch bleeding and its antibacterial properties. Soldiers applied powdered yarrow or fresh yarrow leaves and flowers to stop wounds from bleeding. CLEMATIS Clematis or 威灵仙 (weilingxian) grows vertically on rocky roots as a vine with sparse, four-petal, nodding mauve flowers. Clematis has analgesic, anti-inflammatory, diuretic, and antimicrobial properties and its synergistic nature increases the effectiveness of other herbs. Clematis tea both acts as a vasoconstrictor on brain lining and dilates blood vessels -- it is used to treat headaches and migraines. Externally, a poultice of clematis leaves treats rheumatic pain. Known as “the holy root of the temple” in Chinese medicine, clematis removes wind and dampness, facilitates passage of meridians, and relieves pain. Experimental studies have demonstrated the antirheumatic and analgesic effects of clematis and saponins isolated from clematis may induce apoptosis in breast cancer cells via the mitochondrial pathway. Triterpene saponins from the roots and rhizomes of Clematis mandshurica show inhibitory activity against human colon cancer cell lines. VALERIAN Valerian or 缬草 (xiecao) clings to the rocks nearby. Also known as all-heal, valerian's use as a medicinal herb was documented in ancient Greece. Pliny said that the powder of valerian root given in drink, or the decoction thereof taken, helps all stoppings and stranglings in any part of the body. And Culpeper recommended the root of valerian boiled with licorice, raisins, and aniseed as singularly good for those who are short-winded and for those who are troubled with the cough, to open passages and expectorate phlegm easily. We scratch the root and smell the pungent odor of its chemical constituent valerenic acid. Acting at the central nervous system, valerenic acid and its derivatives have soothing, sedative, spasmolytic, digestive, and hypnotic properties. Physiologically active iridoid valepotriates may cause the release of GABA from nerve endings and block its return to nerve cells, and valerenic acid is known to inhibit an enzyme that destroys GABA. Herbal tea from valerian root has been used for anxiety, tension, hysteria, insomnia, and pain. Valerian root is approved in Europe for mild anxiety and to aid sleep. In Chinese medicine, valerian possesses pungent, bitter, and warm properties and enters through the liver and heart meridians. It acts to induce tranquilization, stop bleeding, and alleviate pain. Valerian root is indicated for irregular menstruation, traumatic injury, back pain, neurasthenia, and indigestion. CORYDALIS Corydalis, also known as golden smoke, scrambled egg, or 延胡索 (yanhusuo), is among the first herbs to flower in spring. An herbal tea of the fumewort corydalis has hypnotic and analgesic properties and is used for stomachache and headache. The Ojibwe people placed the root on coals and inhaled the smoke to clear the head and calm the patient. In Chinese medicine, corydalis invigorates the blood, moves qi, alleviates pain, and reduces masses; thus, it is indicated for pain due to blood stasis and qi stagnation such as epigastric pain and dysmenorrhea. Corydalis contains 20 alkaloids, among them corydaline, tetrahydropalmatine, protopine, and tetrahydrocoptisine, and in laboratory research has exhibited pharmacological action on the central nervous system, including analgesic and sedative effects. Corydalis may block certain receptor sites in the brain, inducing sedation. Its alkaloids may also have cardiovascular effects. Please note: The herb information in this blog is presented for educational purposes only. The use of herbal preparations is not recommended without the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity. Nature's pharmacyJust 24 minutes outside the city of Albuquerque in the East Sandia Mountains of New Mexico, at an elevation of 7420 feet, the wet winter and cold spring have yielded a bounty of herbs. Our guide points out filaree, mullein, hawthorn, dandelion, bear corn, yarrow, clematis, valerian, corydalis, strawberry, wormwood, and verbena among the pines and oaks along the trail. FILAREE
MULLEIN
HAWTHORN
DANDELION
Information in this blog is presented for educational purposes only. Not intended to diagnose, treat, cure, or prevent any disease. The use of herbal preparations is not recommended without seeking the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity.
 September 2019 The U.S. Food and Drug Administration is advising consumers not to purchase or use LOBO, Love in S, Sheaya Lender, and Mero Macho sold and advertised as dietary supplements. FDA has identified an emerging trend in which over-the-counter products, frequently represented as dietary supplements, contain hidden active ingredients that could be harmful. Consumers may unknowingly take products laced with varying quantities of approved prescription drug ingredients, controlled substances, and untested and unstudied pharmaceutically active ingredients. These deceptive products can harm you! LOBO This product promoted for sexual enhancement was identified in an examination of international mail shipments. The red LOBO text and fierce wolf image resemble the mascot of the University of New Mexico, and package copy in Spanish states Maximiza tu potencia sexual – Doble dosis de poder (Maximize your sexual potency – double dose of power). The Food and Drug Administration is advising consumers not to purchase or use LOBO, which contains sildenafil, the active ingredient in the prescription drug Viagra. This undeclared ingredient may interact with nitrates found in some prescription drugs, such as nitroglycerin, and may lower blood pressure to dangerous levels. Mero Macho Mero Macho is sold on the websites fitoterapiausa.com and meromachodrink.com (both sites are currently under construction). FDA laboratory analysis confirmed that Mero Macho contains tadalafil, the active ingredient in the prescription drug Cialis, used to treat erectile dysfunction. Adverse reactions noted in the Cialis prescribing information include headache, indigestion, back pain, myalgia, nasal congestion, flushing, and limb pain. Contraindications are organic nitrates (tadalafil potentiates the hypotensive effect of nitrates), patients with known serious hypersensitivity to tadalafil, and concomitant guanylate cyclase stimulators. People with diabetes, high blood pressure, high cholesterol, or heart disease often take nitrates. Sheaya Lender FDA is advising consumers not to purchase or use Sheaya Lender, a product promoted for weight loss. This product was identified during an examination of international mail shipments. FDA laboratory analysis confirmed that Sheaya Lender contains sibutramine and fluoxetine. Sibutramine is a controlled substance that was removed from the market in October 2010 for safety reasons. This product poses a threat to consumers because sibutramine is known to substantially increase blood pressure and/or heart rate in some people and may present a significant risk for people with a history of coronary artery disease, congestive heart failure, arrhythmia, or stroke. This product may also interact, in life-threatening ways, with other medications a consumer may be taking. Fluoxetine is an FDA-approved drug in a class of drugs called selective serotonin reuptake inhibitors (SSRIs) used for treating depression, bulimia, obsessive-compulsive disorder, panic disorder, and premenstrual dysphoric disorder. The use of SSRIs has been associated with serious side effects including suicidal thinking, abnormal bleeding, and seizures. Ventricular arrhythmia or sudden death can occur when patients are also taking other medications for common conditions (aspirin, ibuprofen, or other drugs for depression, anxiety, bipolar illness, blood clots, chemotherapy, heart conditions, and psychosis). Love in S FDA is advising consumers not to purchase or use Love in S, a product promoted and sold for weight loss. The package has the torso of a fit woman, images of fruits and other plants, and the words “love in S lose inches Natrually.” FDA laboratory analysis confirmed that Love in S contains sibutramine and N-desmethylsibutramine. N-desmethylsibutramine is structurally similar to sibutramine (as described above, sibutramine is a controlled substance that has been removed from the market). “These products are masquerading as dietary supplements — they may look like dietary supplements but they are not legal dietary supplements,” says Michael Levy, director of FDA’s Division of New Drugs and Labeling Compliance. “Some of these products contain hidden prescription ingredients at levels much higher than those found in an approved drug product and are dangerous.” FDA has received numerous reports of harm associated with the use of these products, including stroke, liver injury, kidney failure, heart palpitations, and death. Dietary Supplements and the FDA Dietary supplements, in general, are not FDA-approved. Under the Dietary Supplement Health and Education Act of 1994, dietary supplement firms do not need FDA approval prior to marketing their products. It is the company’s responsibility to make sure its products are safe and that any claims are true. Just because you see a supplement product on a store shelf does NOT mean it is safe or effective. When safety issues are suspected, FDA must investigate and, when warranted, take steps to have the product removed from the market. However, it is much easier for a firm to get a product on the market than it is for FDA to take a product off the market. FDA has worked with the supplement industry to recall numerous products with potentially harmful ingredients including products marketed for weight loss, products marketed for sexual enhancement, and products marketed for body building. The agency has issued warning letters, seized products, and conducted criminal prosecutions. In December 2010, a woman pleaded guilty to an 18-count indictment charging her with the illegal importation and distribution of more than four million diet pills that contained a controlled substance, unapproved drugs, and a possible cancer-causing agent. These hidden ingredients pose a risk to consumer health. Remember, FDA cannot test all products marketed as dietary supplements to identify those containing potentially harmful hidden ingredients. Consumers must be aware of these dangerous products and learn how to identify and avoid them using the warning signs described below. Advice for Consumers What can you do? Be an informed consumer. Know the source of the dietary supplements you buy. Read the label information. Subscribe to FDA notifications informing the public of products marketed as dietary supplements or conventional foods with hidden drug ingredients and chemicals. These products are typically promoted for sexual enhancement, weight loss, and body building and are often represented as being “all natural.” Consumers should exercise caution before purchasing any product in the above categories. “We need consumers to be aware of these dangerous products and to learn how to identify and avoid them,” says Levy. Consumers should look for potential warning signs of tainted products marketed as dietary supplements, such as products claiming to be alternatives to FDA-approved drugs or to have effects similar to prescription drugs, products claiming to be a legal alternative to anabolic steroids, products marketed primarily in a foreign language, products with typographical errors in the label information, or products marketed through mass emails. Beware of sexual enhancement products promising rapid effects, such as working in minutes to hours, or long-lasting effects, such as working for 24 to 72 hours. Generally, if you are using or considering using any product marketed as a dietary supplement, FDA suggests that you check with your healthcare professional or a registered dietician about any nutrients you may need in addition to your regular diet. Ask your healthcare professional for help distinguishing between reliable and questionable information. Ask yourself if it sounds too good to be true. Be cautious if the claims for the product seem exaggerated or unrealistic. Watch out for extreme claims — “quick and effective,” “cure-all,” “can treat or cure diseases,” or “totally safe.” Be skeptical about anecdotal information from personal “testimonials” about incredible benefits or results obtained from using a product. Useful Links FDA’s Medication Health Fraud webpage: https://www.fda.gov/drugs/buying-using-medicine-safely/medication-health-fraud Forms for healthcare professionals and patients to report adverse events or side effects: https://www.accessdata.fda.gov/scripts/medwatch/ Responsibilities of retailers and distributors regarding tainted dietary supplements and foods: https://www.fda.gov/media/79494/download FDA Announcement: Mero Macho All information current as of September 6, 2019. Information in this blog is presented for educational purposes only. Not intended to diagnose, treat, cure, or prevent any disease. The use of herbal preparations is not recommended without seeking the advice of a healthcare provider. Substances in herbal preparations may interact with prescription drugs to eliminate therapeutic efficacy or induce toxicity.
Despite the fact that it is a common condition, postoperative constipation or ileus remains poorly understood and has no established definition, etiology, or treatment. In an attempt to find a solution that quickly restores normal contractile movement of the intestines after surgery, researchers at the University of Texas used a rat model to demonstrate the in vivo and in vitro effects of coffee on gut microbiota and smooth muscle contractility. They fed coffee to rats directly and mixed coffee with gut bacteria in petri dishes. Their findings indicated that coffee suppressed bacteria and increased muscle motility. After the rats were treated with coffee, total bacteria count in feces decreased and the ability of the muscles in the small intestine to contract increased. Xuan-Zheng Shi, lead author of the study, pointed out “Interestingly, these effects are caffeine-independent, because caffeine-free coffee had similar effects as regular coffee.” The investigators in Shi’s study observed changes in bacteria when fecal matter was exposed to coffee in a petri dish and changes in rat feces after the ingestion of different concentrations of coffee over three days. Changes to smooth muscles in the intestine and colon and the response of muscles exposed directly to coffee were documented. Muscles in the lower intestine and colon contracted more readily after a period of coffee ingestion. In petri dishes, the growth of bacteria and other microbes in fecal matter was suppressed when a solution of 1.5 percent coffee was applied and growth slowed further with a 3 percent solution. As Shi noted above, decaffeinated coffee had a similar effect on the microbiome. Researchers have yet to identify the specific mechanism by which coffee increases bowel movement. Further study is necessary to determine whether the decline in total bacteria count in feces helps good bacteria or bad bacteria. Favorable bacteria such as Firmicutes are relatively more efficient at breaking down complex carbohydrates, including cellulose, pectin, and xylan as well as host-derived carbohydrates at the protective mucous layer of the intestine. Increasing the ratio of these bacteria in the gut microbiome leads to higher efficiency in the storage of metabolic byproducts. Additional clinical research is needed to ascertain whether coffee intake is effective for ileus, a temporary arrest of normal contractile movement of the intestines caused by abdominal surgery. A poorly understood postoperative outcome with mechanisms that are neurogenic, inflammatory, and pharmacological in nature, ileus presents significant clinical challenges and lacks effective management strategies. Failure to restore adequate bowel function after surgery causes complications, including infection and intestinal adhesion, which may prolong hospitalization and increase patient distress. Coffee therapy may hold some hope. |
�
AuthorKerilyn Sappington is the founder of Integrative Translations, which specializes in the Chinese to English translation of topics in conventional and complementary medicine. Archives
June 2024
Tags
All
|