Neglected Tropical Diseases: Paragonimiasis and Clonorchiasis
My recent translation work in parasitology
CLONORCHIASIS 华支睾吸虫病
Among the foodborne trematodiases targeted by the World Health Organization, clonorchiasis is a foodborne parasitic disease often caused by contamination from raw or undercooked freshwater fish and shrimp. Clonorchis sinensis 华支睾吸虫 (Chinese liver fluke) is the primary species in the genus Clonorchis known to infect humans and cause clonorchiasis. China has the highest rates of infection and as many as 13 million people may be infected. Clonorchis sinensis parasitizes the bile ducts in the hilar region of the liver, and the International Agency for Research on Cancer classifies Clonorchis sinensis as a Group 1 biological carcinogen contributing to the development of cholangiocarcinoma.
LIFE CYCLE
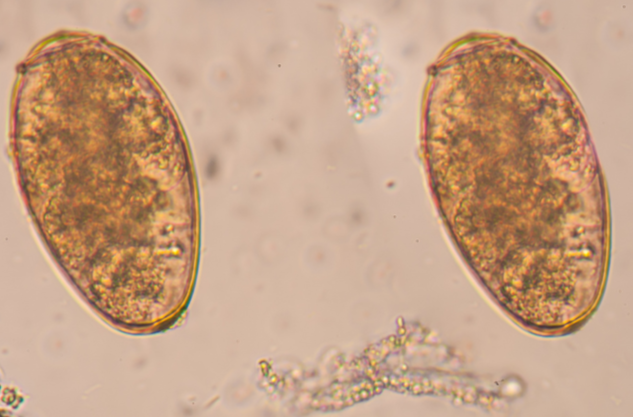
Its life cycle involves two intermediate hosts. The eggs are eaten by the snail and reproduction begins in the soft tissues of the snail. The second intermediate host, freshwater fish, is where the cercariae encyst and develop into infective metacercariae. Infection of humans occurs when people eat raw and undercooked freshwater fish harboring viable metacercariae. Flukes develop first in the duodenum and then migrate to the bile ducts, where they become adults. The adult fluke undergoes self-fertilization and starts to produce eggs. Clonorchis sinensis may survive in the biliary tract for as long as 50 years, producing approximately 2000 eggs per day. These eggs pass with feces, are once again eaten by snails, and the cycle starts anew.
Due to the nonspecific clinical symptoms of clonorchiasis and the lack of awareness among healthcare providers in low endemic areas, often clonorchiasis is only definitively diagnosed when adult flukes are identified during biliary surgery. Endemic areas include China, Japan, Korea, Vietnam and the Amur River Basin in Russia.
SYMPTOMS OF INFECTION
Infection is usually mild and asymptomatic. In severe cases, there may be fever, diarrhea, epigastric pain, hepatomegaly, jaundice, and biliary obstruction. Chronic infection can result in adenocarcinoma of the bile ducts. Invasion of the gallbladder may produce cholecystitis, cholelithiasis, and impaired liver function, as well as liver abscesses.
PREVENTION
Prevention is accomplished by not eating uncooked/undercooked fish and by implementing proper sanitation policies, including the disposal of human, dog, and cat feces in adequately protected sites so that they cannot infect water supplies where the intermediate snail and fish hosts reside.
KEY PUBLIC HEALTH MEASURES AND INSIGHTS
I translated a Chinese report on clonorchiasis surveillance in Xinfeng County, where Clonorchis sinensis infection rates were as high as 14.25% and presented regional clustering. Xinfeng County established a comprehensive demonstration area for the prevention and control of clonorchiasis, with the goal of addressing high infection rates linked to the local custom of consuming raw freshwater fish.
EDUCATION AND PUBLIC AWARENESS CAMPAIGNS Awareness of clonorchiasis notably increased. With the rise in resident knowledge of the disease, infections decreased from 22.5% to 9.7%, although work to increase awareness of the disease and its transmission routes is still needed.
BEHAVIORAL CHANGES Consumption of raw fish decreased and many residents expressed a desire to cease the practice. Willingness to seek treatment after infection also increased.
SURVEILLANCE INSIGHTS Infection rates fluctuated among the villages of Xinfeng County, influenced by gender, age, and level of education. The habit of consuming raw fish persisted among certain segments of the population, underscoring the need for ongoing public health education and interventions.
SAMPLING One administrative village was chosen as a surveillance site to monitor infections in the population. Fecal samples were collected and Clonorchis sinensis eggs counted. The eggs of other parasites were also recorded.
TREATMENT Village doctors assigned by public health centers delivered medication to the homes of those who tested positive for Clonorchis sinensis and coverage of anthelmintic treatments expanded from 69.9% to 89.7% of infected individuals.
The establishment of a demonstration area for the prevention and control of clonorchiasis resulted in a significant reduction in infection rates and a positive shift in public knowledge and behavior associated with the disease. However, the continued presence of risk factors highlights the need for sustained efforts in health education, social and behavior change communication, and treatment programs to further combat clonorchiasis in the region.
TRANSLATED EPIDEMIOLOGICAL REPORTS
Translated reports make it possible for global health agencies to detect trends across linguistic barriers, spot emerging hotspots or shifting transmission zones earlier, accurately document the true global burden of disease, and precisely allocate resources for diagnosis, treatment, prevention, and control.
ADVENT OF NEXT-GENERATION SEQUENCING TECHNOLOGY
Delayed diagnosis means delayed treatment and the use of next-generation sequencing (NGS) technology has been transformative in parasitology, greatly reducing time to diagnose and treat parasitic diseases and eliminating the trial and error of multiple treatments in succession. When a clinic has access to next-generation sequencing, the results pinpoint the parasite and definitive treatment options.
In addition to microscopy and ultrasound, the diagnosis of parasitic disease using MRI and NGS results in earlier diagnosis and treatment. Empiric drug therapy continues to have a role, although NGS allows clinicians to narrow or stop empiric therapy sooner, reducing the unnecessary administration of broad-spectrum antibiotics.
PARAGONIMIASIS 并殖吸虫病
More than 30 species of flukes of the genus Paragonimus 并殖吸虫 have been reported to infect animals and humans. The most common of the species infecting humans is the lung fluke Paragonimus westermani.
LIFE CYCLE
The eggs are excreted unembryonated in sputum or swallowed and passed in stool. In the external environment, the eggs become embryonated and miracidia hatch and seek the first intermediate host (snail) and penetrate its soft tissues. Inside the snail, miracidia develop into sporocysts, rediae, and free-swimming cercariae, which invade the second intermediate host (crab, crayfish, or other crustacean), where they encyst and become metacercariae. Humans become infected when they consume undercooked or raw crab or crayfish harboring the metacercariae of the parasite.
The juvenile fluke hatches in the stomach and follows an extensive migration through the intestinal wall to the abdominal cavity, then through the diaphragm, and finally to the pleural cavity, where it becomes encapsulated and develops into an adult. The flukes may reach the brain and other organs and tissues. Time from infection to oviposition is 65 to 90 days and infections may persist in humans for 20 years.
INVASION AND MIGRATION
In the acute phase, fluke invasion and migration may be marked by diarrhea, abdominal pain, fever, cough, urticaria, hepatosplenomegaly, pulmonary abnormalities, and eosinophilia. Adult flukes in the lungs first produce an inflammatory reaction that results in fever, cough, and increased sputum. Other pulmonary manifestations include hemoptysis and abnormalities in chest imaging. Extrapulmonary locations result in more severe manifestations, especially when the brain is involved.
With progressive destruction of lung tissue, cavitation occurs around the flukes, sputum becomes blood tinged and dark with eggs, and patients experience severe chest pain. The resulting cavity may become secondarily infected with bacteria, and dyspnea, chronic bronchitis, bronchiectasis, and pleural effusion may result. Chronic infections lead to fibrosis in lung tissue.
CEREBRAL PARAGONIMIASIS
Juvenile flukes may invade the spinal cord and brain resulting in severe neurological disease (visual problems, motor weakness, seizures) known as cerebral paragonimiasis.
Although the pathophysiological mechanism of cerebral paragonimiasis is not yet fully understood, it is generally believed that the fluke ascends upward through the mediastinum and along the vascular sheath surrounding the carotid arteries and veins, eventually entering the brain through the foramen lacerum. The parasites localize in the occipital, temporal, and parietal lobes, with occasional cerebellar involvement through invasion of the jugular foramen.
CLINICAL ANALYSIS OF PEDIATRIC CASES
I recently translated a Chinese clinical analysis of 10 cases of cerebral paragonimiasis in children. While relatively rare, cerebral paragonimiasis is more common in children and pediatric anatomy may be a factor – softer tissue, shorter distance for the flukes to migrate.
When children suffer from paragonimiasis, they are more vulnerable to severe or long-term effects due to smaller body size and immature immune system. Because the symptoms of cerebral paragonimiasis – headaches, language and movement disorders, intracranial hemorrhage, and seizures – are nonspecific, the disease is likely to be misdiagnosed initially as viral encephalitis, tuberculous meningoencephalitis, or other intracranial infectious disease. Increased platelet counts and eosinophilia are common and can be intense especially during early migration, so blood routine is crucial for diagnosis. Cranial MRI is an important imaging modality.
In this clinical analysis, all 10 patients were positive for Paragonimus antibodies, providing an evidentiary basis for final diagnosis. Still, vigilance for cross-positivity and false negatives is required. Cerebrospinal fluid test results may not be definitive and a comprehensive approach is essential, so that the results of a single test do not influence final clinical determination. Most patients achieved favorable outcomes after anthelmintic therapy. Surgery was considered only in cases of excessively large lesions or increased intracranial pressure. Close monitoring of signs and symptoms is recommended, along with adjunctive measures to reduce intracranial pressure, control seizures, manage hemorrhage, and support neuroprotection. Cranial MRIs are advised at the end of each course of treatment to assess lesion changes and guide medication use.
PARAGONIMIASIS IS OFTEN UNDERREPORTED
This translation provided important epidemiological data for clinicians and others concerned with the diagnosis and treatment of paragonimiasis. Paragonimiasis is often underreported and misdiagnosed, especially in children, and translated case reports provide clear English data on the diagnosis and treatment of paragonimiasis in China, as well as detailed analysis and guidance for clinicians. Nonspecific symptoms like chronic cough or pleural effusion mimic tuberculosis. Due to language barriers and patchy surveillance, paragonimiasis cases are underestimated in metrics on the global burden of disease. Epidemiological reports improve surveillance, prevent suffering, and enable the effective allocation of global resources. Early treatment means better outcomes, and early information from translated case studies can reduce disability and death. Understanding pediatric cases also enables age-appropriate prevention and education strategies.
The prevalence of paragonimiasis is directly related to consumption of uncooked and undercooked freshwater crabs and crayfish. Education regarding the consumption of uncooked and undercooked freshwater crabs and crayfish is crucial for prevention in endemic areas. Merely pickling and wine soaking crabs and crayfish does not kill the infective metacercarial stage.
CHINESE- ENGLISH PARASITOLOGY TERMS
寄生虫感染 parasitic infection
流行区 endemic area
吸虫 trematode
蠕虫 helminth
并殖吸虫 Paragonimus (lung fluke)
并殖吸虫病 paragonimiasis
华支睾吸虫 Clonorchis sinensis (liver fluke)
华支睾吸虫病 clonorchiasis
肩峰 shoulders
卵壳 eggshell
卵盖 operculum
小疣 abopercular knob
卵内毛蚴 embryonated eggs
中间宿主 intermediate host
毛蚴 miracidium
胞蚴 sporocyst
雷蚴 rediae
尾蚴 cercariae
囊蚴 metacercariae
隧道征 tunnel sign
脑出血 cerebral hemorrhage